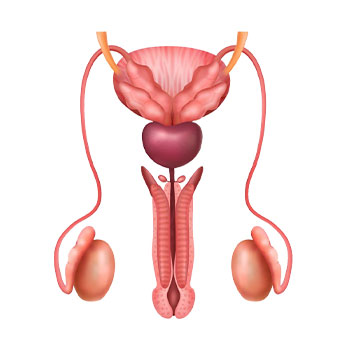
What is Male Infertility?
Male infertility refers to a man's inability to cause pregnancy in a fertile female partner after one year of unprotected intercourse. It is a growing health concern affecting millions of couples worldwide and contributes to approximately 40-50% of all infertility cases. In many instances, male infertility can be diagnosed and treated effectively with the help of a qualified urologist.
Causes of Male Infertility
Male infertility can stem from various factors, including hormonal imbalances, genetic conditions, anatomical problems, or lifestyle habits. Common causes include:
- Low sperm count (oligospermia)
- Varicocele (enlarged veins in the scrotum)
- Erectile dysfunction or ejaculation issues
- Infections or inflammation
- Exposure to radiation, toxins, or heat
- Obesity and unhealthy lifestyle
Understanding Low Sperm Count
Low sperm count, or oligospermia, is one of the most common causes of male infertility. A sperm count below 15 million sperm per milliliter is considered low. This condition reduces the chances of the sperm fertilizing the egg, making conception difficult. Symptoms of low sperm count may not always be obvious, but some men may experience hormonal imbalances, reduced sexual function, or discomfort in the testicles.
The causes of low sperm count can include varicocele, hormonal disorders, infections, undescended testicles, and use of certain medications. Stress, smoking, alcohol consumption, and excessive heat exposure can also negatively affect sperm production.
What is Varicocele?
Varicocele is a condition where the veins within the scrotum become enlarged, similar to varicose veins in the legs. This can cause an increase in temperature in the testicles, impairing sperm production and function. Varicocele is a leading cause of low sperm count and poor sperm quality in men.
While not all varicoceles require treatment, those associated with infertility or discomfort may benefit from surgical intervention.
Microscopic Varicocelectomy – A Modern Treatment Approach
Microscopic varicocelectomy is a precise and minimally invasive surgical technique used to treat varicocele. During this procedure, the urologist uses a high-powered surgical microscope to locate and ligate the affected veins while preserving important structures like arteries and lymphatic vessels.
This advanced surgical method has a high success rate and significantly improves semen quality in many patients. Compared to traditional approaches, microscopic varicocelectomy offers reduced risk of complications, quicker recovery, and minimal scarring.
Diagnosis of Male Infertility
Accurate diagnosis is essential to developing a suitable treatment plan. A comprehensive fertility evaluation typically includes:
- Detailed medical history and physical examination
- Semen analysis to assess sperm count, motility, and morphology
- Scrotal ultrasound to detect varicocele or abnormalities
- Hormonal blood tests
- Genetic testing (if needed)
Timely diagnosis by a qualified specialist can make a significant difference in treatment outcomes.
Meet Dr. Pavan Ganesh Yalavarthi – Male Infertility Specialist in Gudivada
When it comes to male infertility treatment in Gudivada, Dr. Pavan Ganesh Yalavarthi is a trusted name. With extensive experience in urology and male reproductive health, Dr. Yalavarthi offers personalized care to help men overcome infertility challenges. From detailed evaluation to advanced microsurgical procedures like microscopic varicocelectomy, his approach is focused on accuracy, effectiveness, and patient well-being.
If you're searching for a male infertility specialist in Gudivada, Dr. Pavan Ganesh Yalavarthi is dedicated to providing compassionate and evidence-based treatment to restore fertility and improve reproductive outcomes.
Other Treatment Options for Male Infertility
Besides microscopic varicocelectomy, several treatment options are available depending on the underlying cause of infertility:
- Hormonal therapy: For men with hormone imbalances
- Antibiotic treatment: To address infections in the reproductive tract
- Lifestyle modifications: Including weight loss, stopping smoking, and reducing alcohol intake
- Assisted Reproductive Techniques (ART): Such as intrauterine insemination (IUI) or in vitro fertilization (IVF) for cases where natural conception is difficult
When to See a Specialist?
Couples struggling to conceive after a year of regular unprotected intercourse should seek medical advice. It’s also recommended for men who have a known history of varicocele, previous testicular injuries, surgeries, or chronic health issues to consult a urologist early.
Delaying treatment can reduce the chances of successful conception. Consulting a male infertility specialist in Gudivada like Dr. Pavan Ganesh Yalavarthi ensures early detection and timely intervention.
Male infertility can be emotionally and physically challenging, but with the right medical support, many men can regain their fertility. Whether the issue is due to low sperm count or a correctable condition like varicocele, modern treatments offer excellent outcomes. With expert care from Dr. Pavan Ganesh Yalavarthi and advanced options like microscopic varicocelectomy, male infertility treatment in Gudivada is both accessible and effective.
